Scleritis
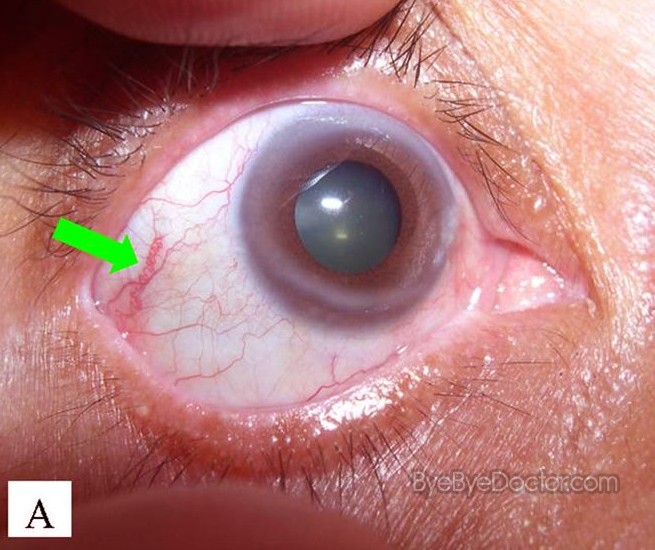
The sclera is the protective outer layer of the eye, which is also the white part of the eye. It’s connected to muscles that help the eye move. About of the eye surface is the sclera.Scleritis is a disorder in which the sclera becomes severely inflamed and red.
Scleritis is typically associated with an autoimmune disorder. Scleritis may also result from trauma to the eye, or, rarely, may be caused by a fungus or a parasite. In other cases the cause is unknow. Scleritis is inflammation of the tough, white structural wall of the eyeball, the sclera. The sclera is made of collagen and is continuous with the cornea, the clear.
It can be very painful. Scleritis is believed to be the result of the body’s immune system overreacting. The type of scleritis you have depends on the location of the inflammation. Most people feel severe pain with the condition, but there are exceptions.Early treatment with medication is necessary to prevent scleritis from progressing. Serious, untreated cases can lead to partial or complete vision loss. Doctors use what’s called the Watson and Hayreh classification to distinguish the different types of scleritis.
Classification is based upon whether the disease is affecting the anterior (front) or posterior (back) of the sclera. The anterior forms are most likely to have an underlying illness as part of their cause.The subtypes of anterior scleritis include:. anterior scleritis: the most common form of scleritis.
nodular anterior scleritis: the second most common form. necrotizing anterior scleritis with inflammation: the most serious form of anterior scleritis. necrotizing anterior scleritis without inflammation: the rarest form of anterior scleritis. posterior scleritis: more difficult to diagnose and detect because it has variable symptoms, including many that mimic other disorders.
Each type of scleritis has similar symptoms, and they can worsen if the condition isn’t treated. Severe eye pain that responds poorly to painkillers is the main symptom of scleritis. Eye movements are likely to make the pain worse.
The pain may spread throughout the entire face, particularly on the side of the affected eye.Other symptoms may include:. excessive tearing, or lacrimation. decreased vision. blurry vision. sensitivity to light, or photophobia. redness of the sclera, or white portion of your eyeThe symptoms of posterior scleritis are not as evident because it does not cause the severe pain as other types. Symptoms include:.
deep-seated headaches. pain caused by eye movement. eye irritation. double visionSome people experience little to no pain from scleritis. This may be because they have:. a milder case. scleromalacia perforans, which is a rare complication of advanced.
a history of using immunosuppressive medications (they prevent activity in the immune system) before symptoms began. Scleritis may occur at any age. Women are more likely to develop it than men. Your doctor will review a detailed medical history and perform an examination and laboratory evaluations to diagnose scleritis.Your doctor may ask questions about your history of systemic conditions, such as whether you’ve had RA, Wegener’s granulomatosis, or IBD. Treatment of scleritis focuses on fighting the inflammation before it can cause permanent damage. Pain from scleritis is also related to inflammation, so reducing the swelling will decrease symptoms.The treatment follows a stepladder approach. If the first step in medication fails, then the second is used.Medications used to treat scleritis include the following:.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are most often used in nodular anterior scleritis. Reducing inflammation also helps to ease scleritis pain.
Corticosteroid pills (such as prednisone) may be used if NSAIDs don’t reduce inflammation. Oral are the preferred choice for posterior scleritis. Immunosuppressive drugs with oral glucocorticoids are preferred for the most dangerous form, which is necrotizing scleritis.
Antibiotics may be used to prevent or treat infections of the sclera. Antifungal medications are commonly used in infections caused by Sjogren’s syndrome.Surgery may also be necessary for severe cases of scleritis.
The process involves the repair of tissues in the sclera to improve muscle function and prevent vision loss.Sclera treatment may also be contingent on treating the underlying causes. For example, if you have an autoimmune disorder, then effectively treating it will help prevent recurring cases of scleritis.
Scleritis can cause significant eye damage, including partial to complete vision loss. When vision loss does occur, it’s usually the result of necrotizing scleritis.
There’s a risk that scleritis will come back despite treatment.Scleritis is a serious eye condition that requires prompt treatment, as soon as symptoms are noticed. Even if your symptoms improve, it’s important to follow up with an ophthalmologist on a regular basis to make sure it doesn’t return. Treating underlying autoimmune conditions that might cause scleritis is also important in preventing future problems with the sclera.
ScleritisInflammation of entire thickness of the scleraScleritis is a serious that affects the white outer coating of the, known as the. The disease is often contracted through association with other diseases of the body, such as. There are three types of scleritis: diffuse scleritis (the most common), nodular scleritis, and necrotizing scleritis (the most severe). Scleritis may be the first symptom of onset of.is inflammation of the, a less serious condition that seldom develops into scleritis. Scleral translucency following recurrent scleritis.Symptoms of scleritis include:. Redness of the sclera and, sometimes changing to a hue.
Severe ocular pain, which may radiate to the temple or jaw. The pain is often described as deep or boring.
and. Decrease in, possibly leading toThe pain of episcleritis is less severe than in scleritis. In hyperemia, there is a visible increase in the blood flow to the sclera , which accounts for the redness of the eye. Unlike in conjunctivitis, this redness will not move with gentle pressure to the conjunctiva.Complications Secondary keratitis or uveitis may occur with scleritis.
The most severe complications are associated with necrotizing scleritis.Pathophysiology Most of the time, scleritis is not caused by an infectious agent. Histopathological changes are that of a chronic granulomatous disorder, characterized by fibrinoid, infiltration by polymorphonuclear cells,.
The surrounded by multinucleated epitheloid giant cells and new vessels, some of which may show evidence of.Diagnosis Scleritis is best detected by examining the sclera in daylight; retracting the lids helps determine the extent of involvement. Other aspects of the eye exam (i.e. Visual acuity testing, slit lamp examination, etc.) may be normal. Scleritis may be differentiated from episcleritis by using or eye drops, which causes blanching of the blood vessels in episcleritis, but not in scleritis.Ancillary tests, and can be helpful, but do not replace the physical examination.Classification Scleritis can be classified as anterior scleritis and posterior scleritis. Anterior scleritis is the most common variety, accounting for about 98% of the cases.
It is of two types: Non-necrotising and necrotising. Non-necrotising scleritis is the most common, and is further classified into diffuse and nodular type based on morphology. Necrotising scleritis accounts for 13% of the cases. It can occur with or without inflammation.Treatment In very severe cases of necrotizing scleritis, eye must be performed to repair damaged in the eye and preserve the patient's vision. For less severe cases, nonsteroidal anti-inflammatory drugs, such as, are prescribed for pain relief. Some patients also benefit from a course of Steroid eye drops such as Scleritis itself is treated with an oral medication containing and an eye solution. In some cases, are prescribed.
Simply using will not treat scleritis. In more aggressive cases of scleritis, chemotherapy (such as systemic immunosuppressive therapy with such drugs as cyclophosphamide or azathioprine) may be used to treat the disease. If not treated, scleritis can cause.Epidemiology Scleritis is not a common disease, although the exact prevalence and incidence are unknown. It is somewhat more common in women, and is most common in the fourth to sixth decades of life.
References. Retrieved 27 November 2012. Bethesda, MD:. Retrieved 20 June 2010. Vorvick, Linda J.
(July 28, 2010). PubMed Health. Retrieved July 6, 2011. ^ Goldman, Lee (2011).
Goldman's Cecil Medicine (24th ed.). Philadelphia: Elsevier Saunders. P. 2440.

Yanoff, Myron; Jay S. Duker (2008). Ophthalmology (3rd ed.). Edinburgh: Mosby.
Pp. 255–261. Maite Sainz de la Maza (Feb 15, 2012). The sclera (2nd ed.). New York: Springer. P. 102. Rosenbaum JT.
The Eye and rheumatic diseases. Zombie catchers cheats. In: Firestein GS, Budd RC, Harris ED Jr, et al., eds. Kelley's Textbook of Rheumatology.
Philadelphia, Pa: Saunders Elsevier; 2008:chap 46. Watson P. Diseases of the sclera and episclera. In: Tasman W, Jaeger EA, eds. Duane’s Ophthalmology.
Philadelphia, Pa: Lippincott Williams & Wilkins; 2009:chap 23.External links Classification.